case reports
June 22, 2022
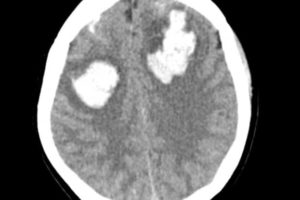
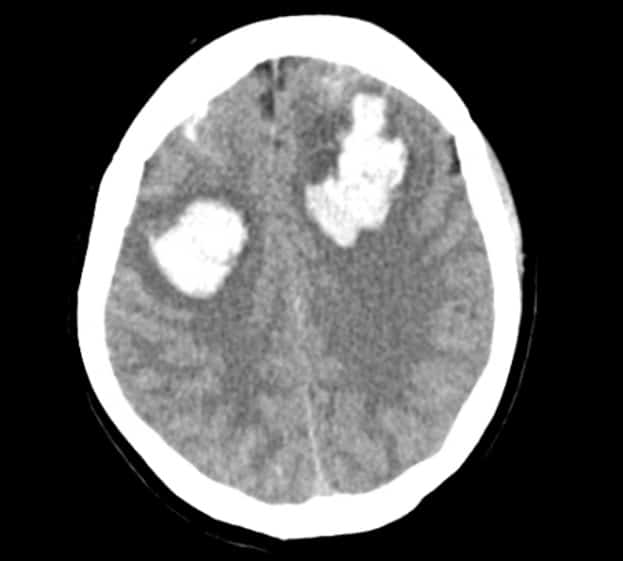
Ecclampsia and its ensuing complications
September 1, 2021
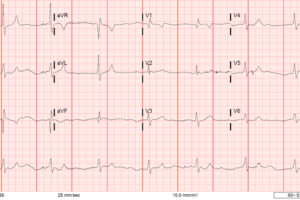
Altered Mental Status in a Patient with an Acute Aortic Dissection
March 21, 2021
Altered mental status at 2 AM: Not always what you think
covid-19

original research

review articles
June 22, 2022
Speed Balls and Their Speed Bumps
September 7, 2021
The Meyering Method
December 18, 2020
COVID-19 Vaccination trial review

physician wellness
November 9, 2022
Protected: MDM
May 14, 2020