50-year-old male presents via EMS from a nursing home after becoming short of breath. The home was concerned because he tested COVID-19 positive the month prior. His other significant history include hypertension, diabetes, psychosis, chronic kidney disease without dialysis, and a history of a trauma that left his paraplegic. EMS noted on scene that patient oxygen saturation was 78% on room air and placed him on 4 L nasal cannula which brought him up to 88% SPO2. History was limited due to patient being non-verbal (stated as baseline). ROS indicates that patient feels fatigue.
Initial Vital signs:
HR: 47 . BP: 80/50. RR: 32. SPO2 saturation 85% on 4LNC.
Physical exam was significant for notable bradycardia, abdominal distention, umbilical hernia. No spontaneous movement of the lower extremities. Patient’s mentation is at baseline per EMS via nursing home.
Clinical course:
Immediately noted the patient’s bradycardia and unstable vital signs. Blood pressure improved with 500cc fluid bolus to 98/67. Cardiac telemetry monitoring was initiated in conjunction with EKG and blood gas.
Arterial Blood Gas: PH: 7.154. PCO2: 53.1. PO2: 79.3 Lactate: 3.1
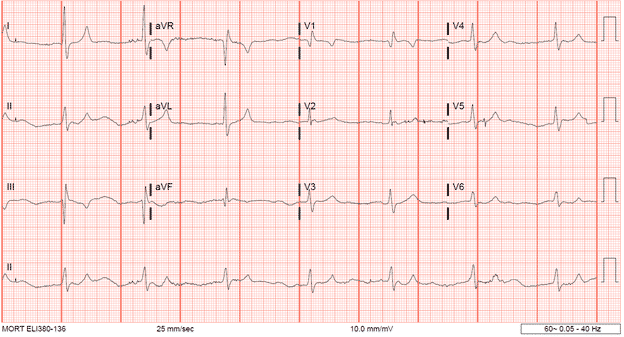
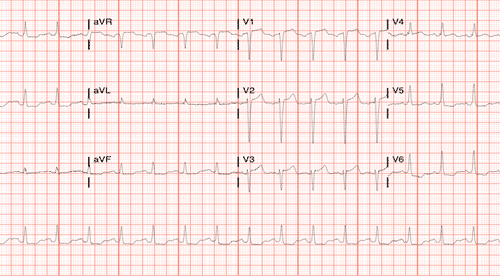
Initial EKG:
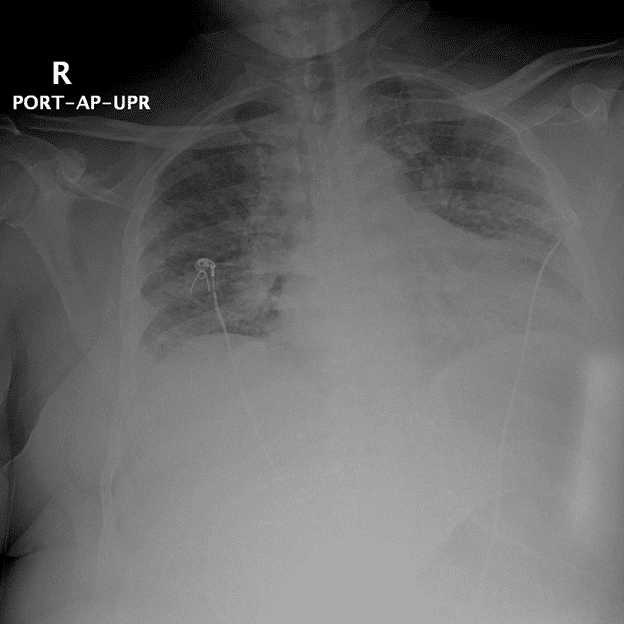
Initial chest x-ray:
CBC resulted: WBC: 9.13. Hgb: 5.5. Platelet Count: 256
During the process of consenting and preparing blood for the patient, the complete metabolic panel returned.
BUN: 103. Creatinine: 5.6. Sodium: 131. Potassium: 9.1
The patient started to become more bradycardic with decreased mentation from initial presentation with increasing respiratory distress. We observed the rhythm strip and saw notable QRS widening. Patient was immediately given a dose of calcium gluconate, albuterol and insulin/dextrose therapy with emergent nephrology consult for dialysis. Patient subsequently went into brief PEA/cardiac arrest and had one round of CPR with subsequent ROSC. Due to increasing oxygen requirement, patient was intubated during the arrest. After initiating insulin/dextrose therapy in addition to the IV calcium along with ACLS measures, the patient reverted to sinus rhythm.
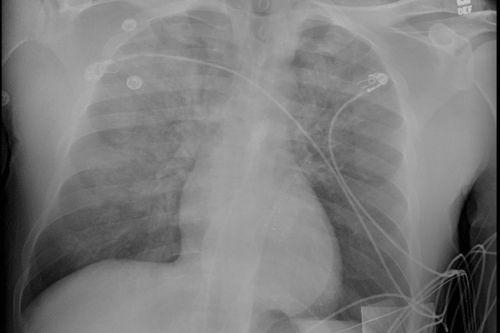
Repeat chest X-ray:
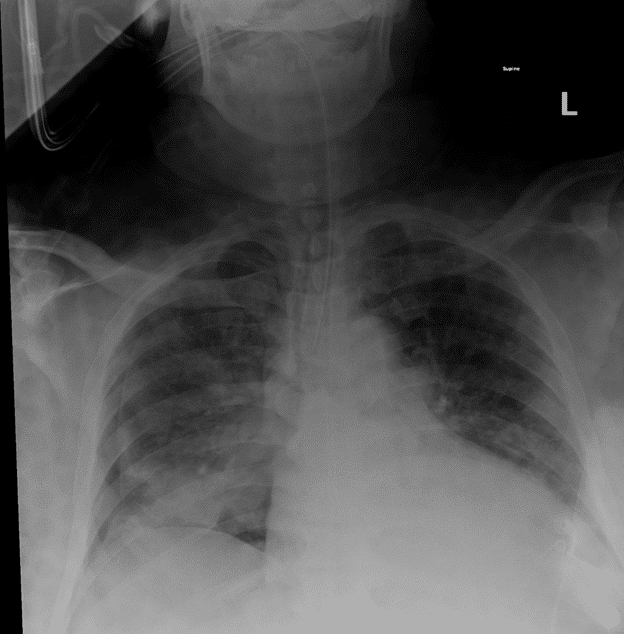
CXR noted a moderate sized pneumothorax after intubation and resuscitation measures were performed. Unclear if related to CPR/arrest or initial progressive respiratory failure. Chest tube was placed, and patient was transferred to the ICU with the presumed diagnosis of pneumonia due to COVID-19 with acute on chronic kidney failure that was exacerbated by severe anemia, hypotension, and COVID-19 infection.
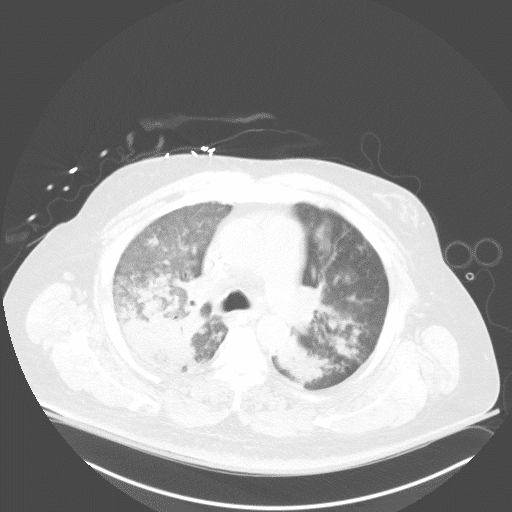
The following CT images were obtained during his stay in the ICU.

After a prolonged stay with treatment, patient was able to be extubated and rehabbed back to his baseline after emergency dialysis and transfusions.
Case Discussion
Hyperkalemia:
Potassium is a major cation in the body with a normal extracellular concentration is 3.5 to 5.0 mEq/L. The kidney is the major player in potassium excretion with it being freely filtered via the renal glomerulus and subsequently reabsorbed in the proximal and ascending tubules with secretion occurring the distal tubules. 4 Hyperkalemia is generally accepted to be >5.5 mEq/L There are many causes of hyperkalemia but generally it is related to intracellular to extracellular shift, increase potassium load, or decrease potassium excretions. For this patient, it was likely due to a combination of acute renal injury resulting in decrease excretion and acidosis resulting in extracellular shift. There have been some observation of COVID-19 resulting in hyperkalemia, likely due to high cell turnover2.
EKG changes are important in hyperkalemia and has been shown to result in a poor prognosis.1 Changes in the EKG results from the dysfunction of membrane polarization. Increase in extracellular potassium results in the resting potential of the excitable myocardium to have a slower and decrease amplitude of action potentials.4 Some sources have try to associate EKG changes with potassium levels as seen below4:
- >5.5 mEq/L:
- Peaked T waves
- 6.5 – 7.5 mEq/L
- Prolonged PR intervals
- Shorten QT interval
- 7.5 – 8.0 mEq/L
- P wave widening and flattening, with eventual disappearance
- QRS widening
- Sinus bradycardia
- Conduction blocks or AV blocks
- 10 – 12 mEq/L
- QRS develops into a Sinusoidal pattern
- Ventricular fibrillation
- Risk for cardiac arrest
The level of hyperkalemia may not manifest as expected. For example, chronic dialyzed patient’s EKG may not manifest signs of hyperkalemia.
Breaking down the patient’s EKG:
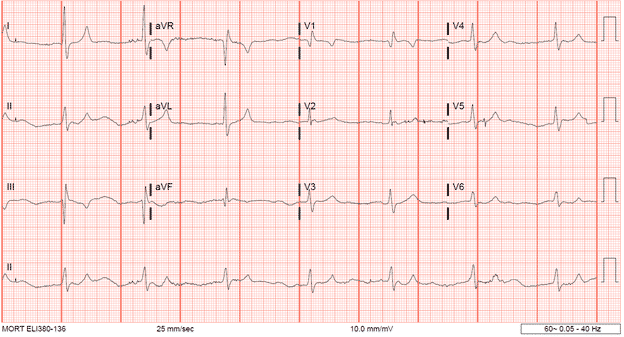
Repolarization abnormalities: Peak T waves in I, aVL,
Signs of paralysis of the atria
- P wave widens and flattens in most leads
- Difficult to decern some P waves
Conduction abnormalities and bradycardia
- Widening of the QRS interval when compared to his EKG from a previous visit (Below)
- Bradycardic (42 BPM)
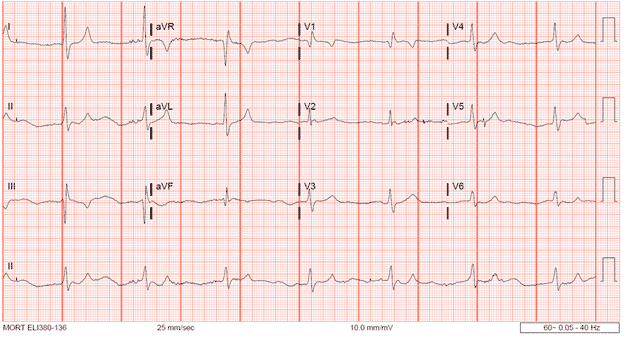
Previous EKG:
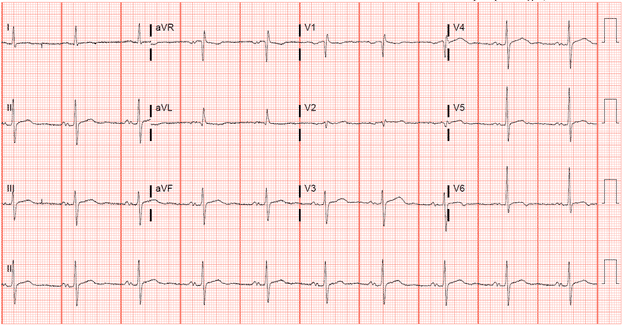
- P waves defined
- Narrow QRS complex
- Rate 60 BPM
Treatment:
In the end, hemodialysis should be considered in any concerning hyperkalemic patient. Other treatment modalities are listed below:
- Membrane stabilization
- Calcium chloride or calcium gluconate
- Shifting potassium into the cells
- Sodium bicarbonate
- Albuterol
- Insulin and glucose
- Potassium Excretion
- Furosemide (renal excretion
- Sodium polystyrene sulfonate (GI excretion)
Case conclusion:
As EM physicians, we are task to tackle multiple problems at once, but should be aware of what may cause the most harm to the patient in the moment. This patient had multiple issues including anemia, hyperkalemia, pneumothorax, and COVID-19, but the hyperkalemia placed the patient at most risk even resulting in an arrest. Despite being a medically complex patient with the COVID-19 virus, he was able to return home after a prolong hospital stay due to the quick actions taken in the ED.
References
- Dépret F, Peacock WF, Liu KD, Rafique Z, Rossignol P, Legrand M. Management of hyperkalemia in the acutely ill patient. Ann Intensive Care. 2019;9(1):32. Published 2019 Feb 28. doi:10.1186/s13613-019-0509-8
- Gupta, A., Madhavan, M.V., Sehgal, K. et al. Extrapulmonary manifestations of COVID-19. Nat Med 26, 1017–1032 (2020). https://doi.org/10.1038/s41591-020-0968-3
- Huis in ‘t Veld MA, Mattu A, Thurman R. Hyperkalemia. In: Knoop KJ, Stack LB, Storrow AB, Thurman R. eds. The Atlas of Emergency Medicine, 5e. McGraw-Hill; Accessed October 13, 2020. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=2969§ionid=250463371
- Petrino R, Marino R. Fluids and Electrolytes. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw-Hill; Accessed October 13, 2020. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=2353§ionid=218687466
- Ritchie JV, Juliano ML, Thurman R. ECG ABNORMALITIES. In: Knoop KJ, Stack LB, Storrow AB, Thurman R. eds. The Atlas of Emergency Medicine, 4e. McGraw-Hill; Accessed October 13, 2020. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=1763§ionid=125438683


This Post Has 0 Comments