History: Patient is a 52 y/o M with PMH of DM2 who presented for hip pain for 2 months, worsening over the past 2 weeks. Patient initially reported that he was at work 2 hours prior when he developed sudden onset, severe, right sided hip pain. Denied trauma or falling. Patient denied fevers, abdominal pain, nausea, vomiting, rectal bleeding, weight loss, night sweats or diarrhea but did endorse non-localized chest pain that was associated with non-exertional shortness of breath. Patient was not having any chest pain at present however. The patient was noted to have a history of poor glycemic control and medication compliance in regards to insulin therapy for DM.
Vital signs:
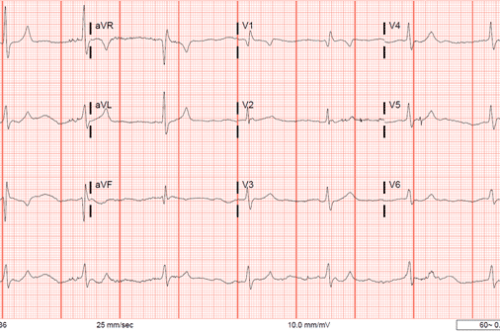
HR 149, BP 95/59, T 98 F (36.7C), RR 26, SPO2 99% RA.
Physical Exam:
CV/Resp: notable for tachycardia with regular rhythm, mildly tachypneic with not increased WOB
Abdomen: soft, nondistended, non-tender, no rebound or guarding
Extremities: large, firm mass noted to right gluteal region, no overlying skin changes, no fluctuance, crepitus or surrounding cellulitis, ROM of hip limited due to patient pain
Labs:
CBC: WBC count 18.25, H/H: 10.0/30.8, Plt: 579k, Bands: 7
CMP: Cr 1.0, Glucose: 565, CO2 21, Na 122, AG 12.
Troponin: <0.015
Lactate: 4.0
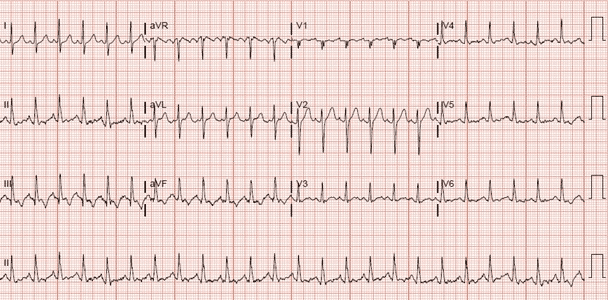
EKG:
The patient was initiated as a ‘sepsis alert’ and resuscitation measures were initiated with empiric broad spectrum antibiotics and IVF. CT scanning was performed of the chest/abdomen/pelvis as well as blood and urine cultures to evaluate for source of infection.
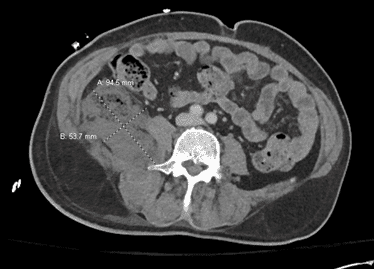
CT of the abdomen/pelvis
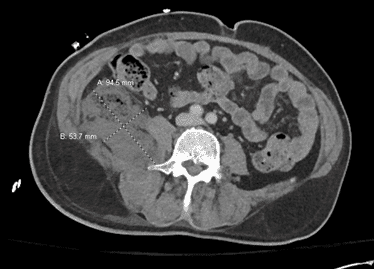
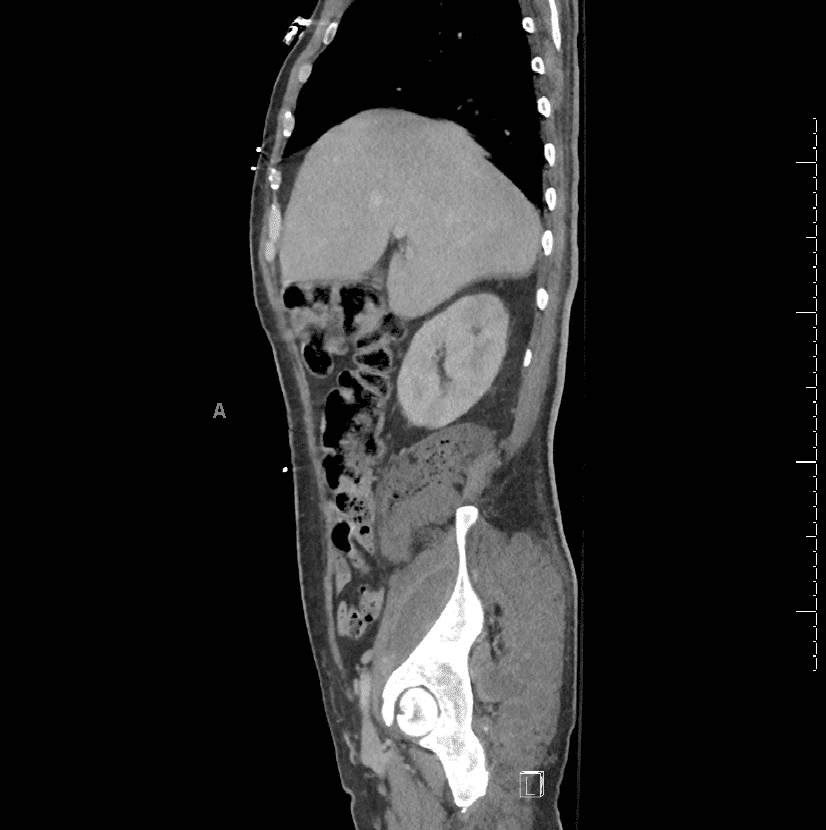
CT of the abdomen/pelvis displayed an extensive complex mixed air and fluid collection of the right hemipelvis and gluteal musculature. Abnormal appearing SI joint which was thought to represent seeding or sequelae of septic emboli. Additional considerations were also for right SI joint septic arthritis with surrounding intramuscular abscess formation and possibly findings could also represent ruptured colonic neoplasm with superimposed infection and abscess formation.
CT Chest
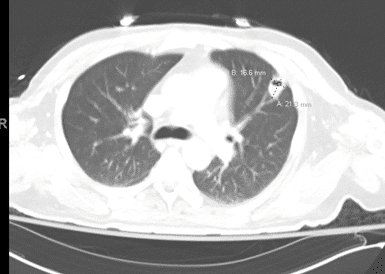
CT of the chest displayed a small cavitary lesion of the left lingula, 2.1×1.7cm
Clinical Course:
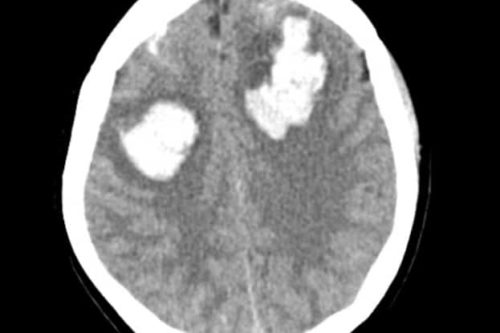
The patient was found to have septic shock secondary to MSSA bacteremia with right sided iliopsoas abscess, retroperitoneal abscess, and gluteal abscess extension of the psoas abscess. Initially there was concern for perforated colon causing enterococcal infection causing the abscess extension and exploratory laparotomy was performed. Ex-lap did not show any significant colon pathology or involvement. Due to multiple abscesses, there was concern for septic emboli thus TEE was performed that displayed no vegetative valve disease, or ejection fraction abnormality. The pulmonary cavitary mass was thought secondary to septic emboli and not mycobacterium. The patient was treated in the surgical ICU and underwent further incision and drainage of the gluteal extension component with drainage of retroperitoneal abscess augmented by drains placed by Interventional Radiology. An Abscessogram performed showed a sinus fistula tract to the gluteal musculature via the sciatic notch. Subsequently wound care was augmented with wound vac devices. The patient was also noted to have pyelonephritis likely secondary to uncontrolled DM and bacteremia and remained on strict I&O throughout the hospital course with clinical improvement. The patient’s total hospital stay was 12 days. The patient was discharged on oral antibiotics and outpatient wound care.
The patient returned one month later with back pain and increased drainage from the gluteal wound site. He was found to have osteomyelitis of the L3 vertebrae by aspiration biopsy and required additional incision and drainage of the gluteal wound as well as IV antibiotics for osteomyelitis. Blood cultures again returned with MSSA and the patient was placed on long term IV infusion of nafcillin on discharge. Total admission at that time was 11 days.
The patient returned to the ED 10 days later for right sided shoulder pain and was found to have septic arthritis again colonized by MSSA and bacillus sp. The hip wound vac was found to be malfunctioning and extension from hematogenous spread was thought to cause the septic arthritis. The patient underwent arthrocentesis of the right shoulder joint by orthopedics and revision of the gluteal drains by IR/General surgery. The patient had a PICC line revised and was discharged subsequently on 4 additional weeks of IV nafcillin infusion. The patient underwent gluteal drain removal after 4 weeks and was noted to be improved although was left with chronic hip pain.
Case Discussion:
Psoas Abscesses are rare and were often diagnosed postmortem prior to the advent of the CT. (2) “The psoas muscle arises from the transverse processes and the lateral aspects of the vertebral bodies between the 12th thoracic and the 5th lumbar vertebrae. From this origin, it courses downward across the pelvic brim, passes deep to the inguinal ligament and anterior to the hip joint capsule to form a tendon that inserts into the lesser trochanter of the femur. The iliacus muscle joins the psoas to insert via the same tendon. The iliacus and psoas muscles typically function as the main hip flexors.
Psoas Abscesses are described as either primary or secondary.
Primary abscesses are the result of lymphatic seeding or hematogenous spread (2-4). Affected patients are often immunosuppressed (DM, HIV, ESRD, IVDU). Most common in children and young adults (2,3,6). Most commonly due to Staphylococcus Aureus (3,6,12,18,25, 26).
Secondary abscesses are the result of direct spread from adjacent structures (vertebra, hip, GI, GU, Aorta) (1-3, 6, 8-22, 24).More commonly polymicrobial, often enteric organisms. (3,6)
Presentation is often with fever, limping, flank or back pain often with radiation to the hip. (1-3,6, 12,23,41) Labs often show elevated inflammatory markers and leukocytosis. (2,6,12, 28) Treatment includes IV antibiotics and abscess drainage either with IR or open. (1,2,3, 18,41, 54,59) Antibiotics should be based on culture data, however, if empiric antibiotics are started they should cover S. Aureus (including MRSA) and enteric organisms. (41)
Reviewing this case, psoas abscesses unless recognized early can result in significant morbidity and downstream complications.
References
- Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J 2004; 80:459.
- Mückley T, Schütz T, Kirschner M, et al. Psoas abscess: the spine as a primary source of infection. Spine (Phila Pa 1976) 2003; 28:E106.
- Ricci MA, Rose FB, Meyer KK. Pyogenic psoas abscess: worldwide variations in etiology. World J Surg 1986; 10:834.
- Santaella RO, Fishman EK, Lipsett PA. Primary vs secondary iliopsoas abscess. Presentation, microbiology, and treatment. Arch Surg 1995; 130:1309.
- Aota Y, Onari K, Suga Y. Iliopsoas abscess and persistent radiculopathy: a rare complication of continuous infusion techniques of epidural anesthesia. Anesthesiology 2002; 96:1023.
- Navarro López V, Ramos JM, Meseguer V, et al. Microbiology and outcome of iliopsoas abscess in 124 patients. Medicine (Baltimore) 2009; 88:120.
- Gruenwald I, Abrahamson J, Cohen O. Psoas abscess: case report and review of the literature. J Urol 1992; 147:1624.
- Buttaro M, González Della Valle A, Piccaluga F. Psoas abscess associated with infected total hip arthroplasty. J Arthroplasty 2002; 17:230.
- Lee BB, Ngan Kee WD, Griffith JF. Vertebral osteomyelitis and psoas abscess occurring after obstetric epidural anesthesia. Reg Anesth Pain Med 2002; 27:220.
- Dolfin D, Barkin J, Arenson AM, Herschorn S. Psoas abscess after operation on lumbar spine. Urology 1983; 21:544.
- Lin SS, Vaccaro AR, Reisch S, et al. Low-velocity gunshot wounds to the spine with an associated transperitoneal injury. J Spinal Disord 1995; 8:136.
- Lin MF, Lau YJ, Hu BS, et al. Pyogenic psoas abscess: analysis of 27 cases. J Microbiol Immunol Infect 1999; 32:261.
- Alpantaki K, Papoutsidakis A, Katonis P, Hadjipavlou A. Vertebral osteomyelitis, epidural and psoas abscess after epidural catheter use. Acta Orthop Belg 2007; 73:670.
- Maron R, Levine D, Dobbs TE, Geisler WM. Two cases of pott disease associated with bilateral psoas abscesses: case report. Spine (Phila Pa 1976) 2006; 31:E561.
- Dauchy FA, Dupon M, Dutronc H, et al. Association between psoas abscess and prosthetic hip infection: a case-control study. Acta Orthop 2009; 80:198.
- Gordin F, Stamler C, Mills J. Pyogenic psoas abscesses: noninvasive diagnostic techniques and review of the literature. Rev Infect Dis 1983; 5:1003.
- Ogihara M, Masaki T, Watanabe T, et al. Psoas abscess complicating Crohn’s disease: report of a case. Surg Today 2000; 30:759.
- Yacoub WN, Sohn HJ, Chan S, et al. Psoas abscess rarely requires surgical intervention. Am J Surg 2008; 196:223.
- Hsu RB, Lin FY. Psoas abscess in patients with an infected aortic aneurysm. J Vasc Surg 2007; 46:230.
- Inufusa A, Mikawa Y, Morita I, Fujiwara T. Ruptured abdominal aortic aneurysm associated with a psoas abscess. Arch Orthop Trauma Surg 2002; 122:306.
- Sharif MA, Lee B, Lau LL, et al. Prosthetic stent graft infection after endovascular abdominal aortic aneurysm repair. J Vasc Surg 2007; 46:442.
- Klonaris C, Vourliotakis G, Katsargyris A, et al. Primary aortoduodenal fistula without abdominal aortic aneurysm in association with psoas abscess. Ann Vasc Surg 2006; 20:541.
- Lee YT, Lee CM, Su SC, et al. Psoas abscess: a 10 year review. J Microbiol Immunol Infect 1999; 32:40.
- Alan C, Ataus S, Tunç B. Xanthogranulamatous pyelonephritis with psoas abscess: 2 cases and review of the literature. Int Urol Nephrol 2004; 36:489.
- Flavin NE, Gomez M. Fever, pain, and a limp: a case of a psoas and spinal epidural abscess caused by methicillin-resistant Staphylococcus aureus in a diabetic patient. J Natl Med Assoc 2009; 101:84.
- De U, Pal DK. Seventy cases of non-tubercular psoas abscess at a rural referral centre in South Bengal. Trop Doct 2006; 36:53.
- Ulu-Kilic A, Karakas A, Erdem H, et al. Update on treatment options for spinal brucellosis. Clin Microbiol Infect 2014; 20:O75.
- Chang CM, Ko WC, Lee HC, et al. Klebsiella pneumoniae psoas abscess: predominance in diabetic patients and grave prognosis in gas-forming cases. J Microbiol Immunol Infect 2001; 34:201.
- Giladi M, Sada MJ, Spotkov J, Bayer AS. Pneumococcal psoas abscess: report of a case and review of the world literature. Isr J Med Sci 1996; 32:771.
- Dubois D, Robin F, Bouvier D, et al. Streptobacillus moniliformis as the causative agent in spondylodiscitis and psoas abscess after rooster scratches. J Clin Microbiol 2008; 46:2820.
- Tamargo Delpón M, Demelo-Rodríguez P, Cano Ballesteros JC, Vela de la Cruz L. [Psoas abscess caused by Staphylococcus lugdunensis]. Rev Argent Microbiol 2016; 48:119.
- Palavutitotai N, Chongtrakoo P, Ngamskulrungroj P, Chayakulkeeree M. NOCARDIA BEIJINGENSIS PSOAS ABSCESS AND SUBCUTANEOUS PHAEOHYPHOMYCOSIS CAUSED BY PHAEOACREMONIUM PARASITICUM IN A RENAL TRANSPLANT RECIPIENT: THE FIRST CASE REPORT IN THAILAND. Southeast Asian J Trop Med Public Health 2015; 46:1049.
- Heyd J, Meallem R, Schlesinger Y, et al. Clinical characteristics of patients with psoas abscess due to non-typhi Salmonella. Eur J Clin Microbiol Infect Dis 2003; 22:770.
- Aoyama M, Nemoto D, Matsumura T, Hitomi S. A fatal case of iliopsoas abscess caused by Salmonella enterica serovar Choleraesuis that heterogeneously formed mucoid colonies. J Infect Chemother 2015; 21:395.
- Bozbaş GT, Ünübol Aİ, Gürer G. Seronegative brucellosis of the spine: A case of psoas abscess secondary to brucellar spondylitis. Eur J Rheumatol 2016; 3:185.
- Galy A, Decousser JW, El-Anbassi S, et al. Psoas abscess and chronic Q fever: a contiguous or hematogenous complication? A case report and literature review. Infect Dis (Lond) 2016; 48:626.
- Teijido J, Drendel AL. Disseminated Blastomycosis in a Teenager Presenting with Pleural Effusion and Splenomegaly. J Emerg Med 2019; 56:e23.
- Leeman M, Burgers P, Brehm V, van Brussel JP. Psoas abscess after bacille Calmette-Guérin instillations causing iliac artery contained rupture. J Vasc Surg 2017; 66:1236.
- Diaco ND, Strohdach B, Falkowski AL, et al. Psoas Abscess Due to Mycobacterium avium in A Patient with Chronic Lymphocytic Leukemia-Case Report and Review. J Clin Med 2019; 8.
- Han YM, Kim AY, Lim RK, et al. Neonatal Iliopsoas Abscess: The First Korean Case. J Korean Med Sci 2015; 30:1203.
- Huang JJ, Ruaan MK, Lan RR, Wang MC. Acute pyogenic iliopsoas abscess in Taiwan: clinical features, diagnosis, treatments and outcome. J Infect 2000; 40:248.
- Bresee JS, Edwards MS. Psoas abscess in children. Pediatr Infect Dis J 1990; 9:201.
- Stefanich RJ, Moskowitz A. Hip flexion deformity secondary to acute pyogenic psoas abscess. Orthop Rev 1987; 16:67.
- Fish DE, Middleton K, Gluzman A. Atypical presentation of osteomyelitis, discitis, epidural, and iliopsoas abscess in diffuse idiopathic skeletal hyperostosis (DISH) syndrome. Am J Phys Med Rehabil 2008; 87:960.
- Deng Y, Zhang Y, Song L, et al. Primary iliopsoas abscess combined with rapid development of septic shock: Three case reports. Medicine (Baltimore) 2018; 97:e13628.
- Arai Y, Kawakami T, Soga H, Okada Y. Psoas abscess associated with iliac vein thrombosis and piriformis and gluteal abscesses. Int J Urol 1999; 6:257.
- Ijaz M, Sakam S, Ashraf U, Marquez JG. Unusual Presentation of Recurrent Pyogenic Bilateral Psoas Abscess Causing Bilateral Pulmonary Embolism by Iliac Vein Compression. Am J Case Rep 2015; 16:606.
- Volpin A, Kini SG, Berizzi A. Psoas muscle pyogenic abscess in association with infected hip arthroplasty: a rare case of simultaneous bilateral presentation. BMJ Case Rep 2015; 2015.
- Zissin R, Gayer G, Kots E, et al. Iliopsoas abscess: a report of 24 patients diagnosed by CT. Abdom Imaging 2001; 26:533.
- Takada T, Terada K, Kajiwara H, Ohira Y. Limitations of using imaging diagnosis for psoas abscess in its early stage. Intern Med 2015; 54:2589.
- Lee JK, Glazer HS. Psoas muscle disorders: MR imaging. Radiology 1986; 160:683.
- Kao PF, Tzen KY, Tsui KH, et al. The specific gallium-67 scan uptake pattern in psoas abscesses. Eur J Nucl Med 1998; 25:1442.
- Kimizuka Y, Ishii M, Murakami K, et al. A case of skeletal tuberculosis and psoas abscess: disease activity evaluated using (18) F-fluorodeoxyglucose positron emission tomography-computed tomography. BMC Med Imaging 2013; 13:37.
- Kishi Y, Kajiwara S, Seta S, et al. Retroperitoneal schwannoma misdiagnosed as a psoas abscess: report of a case. Surg Today 2002; 32:849.
- Wang B, Liu W, Shao Z, Zeng X. Retroperitoneal metastatic poorly differentiated carcinoma with β-human chorionic gonadotropin secretion presenting as a psoas abscess: A case report and review of the literature. Medicine (Baltimore) 2017; 96:e6837.
- Menon A, Agashe VM, Jakkan MS. Rare Case of Iliopsoas Abscess Secondary to Mucinous Adenocarcinoma of the Colon: A Case Report. J Orthop Case Rep 2018; 8:32.
- Oliosi E, Pointeau O, Dacheux C, et al. [A muscular calcium pyrophosphate deposition pseudo-abscess: An atypical localization of chondrocalcinosis]. Rev Med Interne 2019; 40:211.
- Simonin A, Paris O, Brouland JP, et al. Degenerative Disc Disease Mimicking Spondylodiscitis with Bilateral Psoas Abscesses. World Neurosurg 2018; 120:43.
- Dave BR, Kurupati RB, Shah D, et al. Outcome of percutaneous continuous drainage of psoas abscess: A clinically guided technique. Indian J Orthop 2014; 48:67.
- Atkin G, Qurashi K, Isla A. Laparoscopic drainage of bilateral tuberculous psoas abscesses. Surg Laparosc Endosc Percutan Tech 2005; 15:380.
- Hsieh MS, Huang SC, Loh el-W, et al. Features and treatment modality of iliopsoas abscess and its outcome: a 6-year hospital-based study. BMC Infect Dis 2013; 13:578.
- Sherman SJ, Stern J, Neufeld P. Recurrent psoas abscess. Postgrad Med 1987; 81:96, 99.



This Post Has 0 Comments